Multisystem involvement may be a sign of ATTR
ATTR develops primarily due to the accumulation of amyloid deposits in the heart and other tissues of the body.1-4
- As the disease progresses, multisystem involvement may develop and should be considered a red flag5,6
- Red-flag symptoms can aid in raising clinical suspicion5,6
- A single screening result cannot establish a diagnosis, but may be a warning sign of ATTR
- Unexplained left ventricular (LV) wall thickening in the absence of hypertension
- Conduction system disease/atrial fibrillation
- Aortic stenosis
- HFpEF in combination with other noncardiac red-flag symptoms
- Intolerance/suboptimal response to common cardiovascular medications, including HF treatments*
- Elevated NT-proBNP and troponin
- Shortness of breath
- Edema
*Patients with ATTR-CM can have intolerance to standard medications for heart failure, including ARNi, ACEi, ARB, or β blockers.
ACEi=angiotensin-converting enzyme inhibitor; ARB=angiotensin receptor blocker;
ARNi=angiotensin receptor-neprilysin inhibitor; ATTR-CM=cardiomyopathy of transthyretin-mediated amyloidosis; echo=echocardiography; EKG=electrocardiography; cMRI=cardiac magnetic resonance imaging; HF=heart failure; HFpEF=heart failure with preserved ejection fraction; NT-proBNP=N-terminal prohormone of brain type natriuretic peptide.
- Altered sensation
- Difficulty walking
- Muscle weakness
- Numbness and tingling
- Autonomic nervous system disruptions (eg, GI symptoms, orthostatic hypotension, recurrent UTIs, sexual dysfunction)
GI=gastrointestinal; UTI=urinary tract infection.
- Bilateral carpal tunnel syndrome
- Lumbar spinal stenosis
- Biceps tendon rupture
- Rotator cuff injury
- Trigger finger
- Vitreous opacification
- Glaucoma
- Abnormal conjunctival vessels
- Pupillary abnormalities
- Proteinuria
- Renal failure
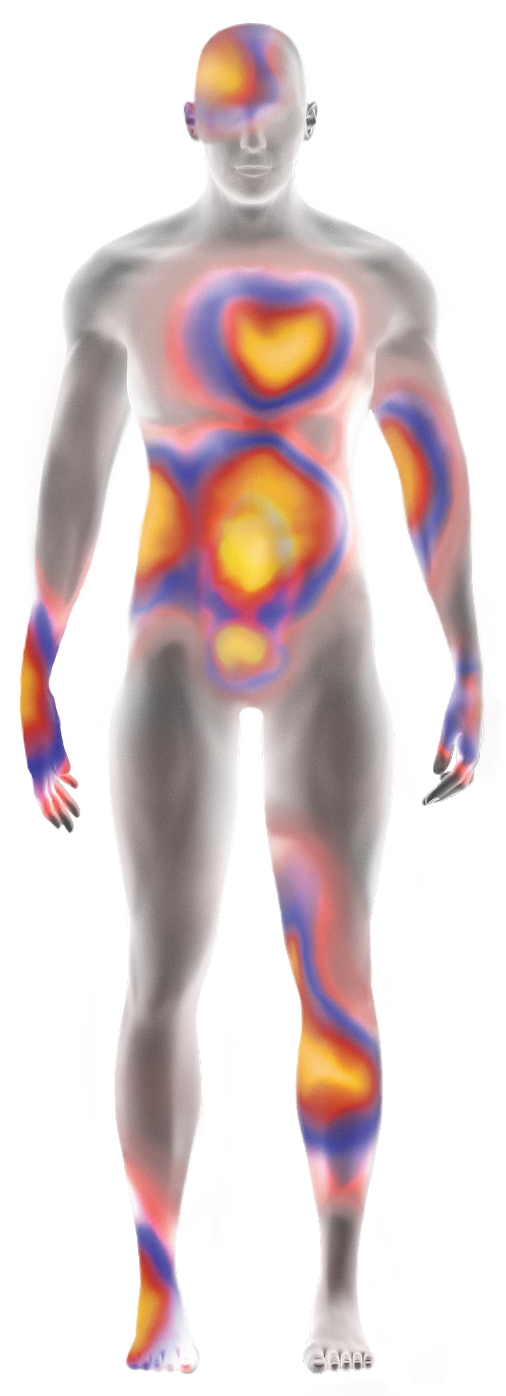
Patients with ATTR experience increasing burden of disease across multiple organ systems as the disease progresses.6,7,15,19
ATTR=transthyretin-mediated amyloidosis.
References:
- Koike H, et al. Biomedicines. 2019;7(1):11.
- Adams D, et al. Neurology. 2015;85(8):675-682.
- Adams D, et al. Curr Opin Neurol. 2016;29(suppl 1):S14-S26.
- Mohty D, et al. Arch Cardiovasc Dis. 2013;106(10):528-540.
- Garcia-Pavia P, et al. Rev Esp Cardiol. 2025;78(4):301-310.
- Kittleson MM, et al. J Am Coll Cardiol. 2023;81(11):1076-1126.
- Kittleson MM, et al. Circulation. 2020;142(1):e7-e22.
- Maurer MS, et al. Circ Heart Fail. 2019;12(9):e006075.
- González-López E, et al. Eur Heart J. 2015;36(38):2585-2594.
- Maloberti A, et al. Int J Cardiol Cardiovasc Risk Prev. 2024;21:200271.
- Dharmarajan K, et al. J Am Geriatr Soc. 2012;60(4):765-774.
- Castaño A, et al. Eur Heart J. 2017;38(38):2879-2887.
- Witteles RM, et al. JACC Heart Fail. 2019 Aug;7(8):709-716.
- Conceição I, et al. J Peripher Nerv Syst. 2016;21(1):5-9.
- Nativi-Nicolau JN, et al. Heart Fail Rev. 2022;27(3):785-793.
- Brito D, et al. Glob Heart. 2023;18(1):1-47.
- Mitter SS, et al. ISA Congress 2020. Poster PT135.
- Maurer MS, et al. J Am Coll Cardiol. 2016;68(2):161-172.
- Rozenbaum MH, et al. Cardiol Ther. 2021;10(1):141-159.